Blue Cross Blue Shield Appeal Form
Blue Cross Blue Shield Appeal Form - With the form, the provider may attach supporting medical information and mail to the following address within the required time. Web claim review and appeal. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. Do not use this form for dental appeals. It is provided as a general resource to providers regarding the types of claim reviews and appeals that may be available for commercial and medicaid claims. To help you prepare your reconsideration request, you may arrange with us to provide a copy, free of charge, of all relevant materials, and plan documents under our control relating to your claim, including those that involve any expert review(s) of your claim. If you have questions about a form you need, call the customer service number on the back of your member id card. If you're a blue cross blue shield of michigan member and are unable to resolve your concern through customer service, we have a formal grievance and appeals process. The following information does not apply to medicare advantage and hmo claims. The centers for medicare & medicaid services (cms) has developed forms for use by all blue cross medicare advantage prescribing doctors and members.
These forms can be used for coverage determinations, redeterminations and appeals. Send only one appeal form per claim. Web provider appeal form please complete the following information and return this form with supporting documentation to the applicable address listed on the corresponding appeal instructions. Web here are some common forms you may need to use with your plan. With the form, the provider may attach supporting medical information and mail to the following address within the required time. The centers for medicare & medicaid services (cms) has developed forms for use by all blue cross medicare advantage prescribing doctors and members. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. Web forms to use to request determinations and file appeals. If you're a blue cross blue shield of michigan member and are unable to resolve your concern through customer service, we have a formal grievance and appeals process. Some health plans have customized forms that are not listed on this page.
Web forms to use to request determinations and file appeals. To help you prepare your reconsideration request, you may arrange with us to provide a copy, free of charge, of all relevant materials, and plan documents under our control relating to your claim, including those that involve any expert review(s) of your claim. These forms can be used for coverage determinations, redeterminations and appeals. Web appeal form who is this for? Send only one appeal form per claim. Some health plans have customized forms that are not listed on this page. If you have questions about a form you need, call the customer service number on the back of your member id card. The centers for medicare & medicaid services (cms) has developed forms for use by all blue cross medicare advantage prescribing doctors and members. Web provider appeal form please complete the following information and return this form with supporting documentation to the applicable address listed on the corresponding appeal instructions. Web claim review and appeal.
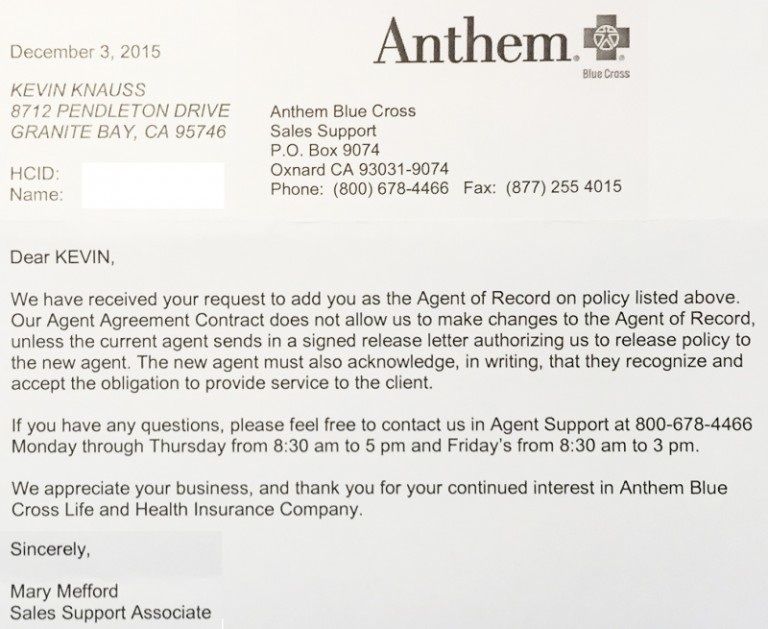
Anthem Blue Cross denies Covered California consumers agent
If you're a blue cross blue shield of michigan member and are unable to resolve your concern through customer service, we have a formal grievance and appeals process. You can file a complaint by phone or ask for a complaint form to be mailed to you. Need medicare forms or documents? Web level i provider appeals for billing/coding disputes and.
Blue Cross Blue Shield Appeal Form / Fitness Benefit Form Blue Cross
It is provided as a general resource to providers regarding the types of claim reviews and appeals that may be available for commercial and medicaid claims. You can file a complaint by phone or ask for a complaint form to be mailed to you. Web section 8 of the blue cross and blue shield service benefit plan brochure. Send only.
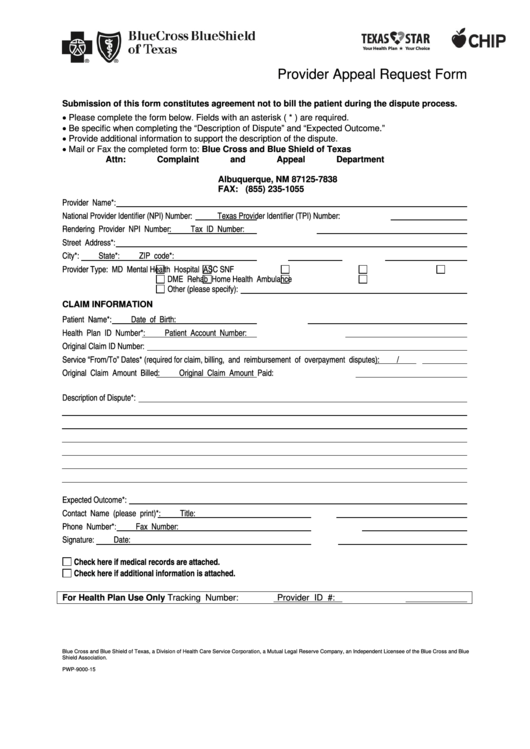
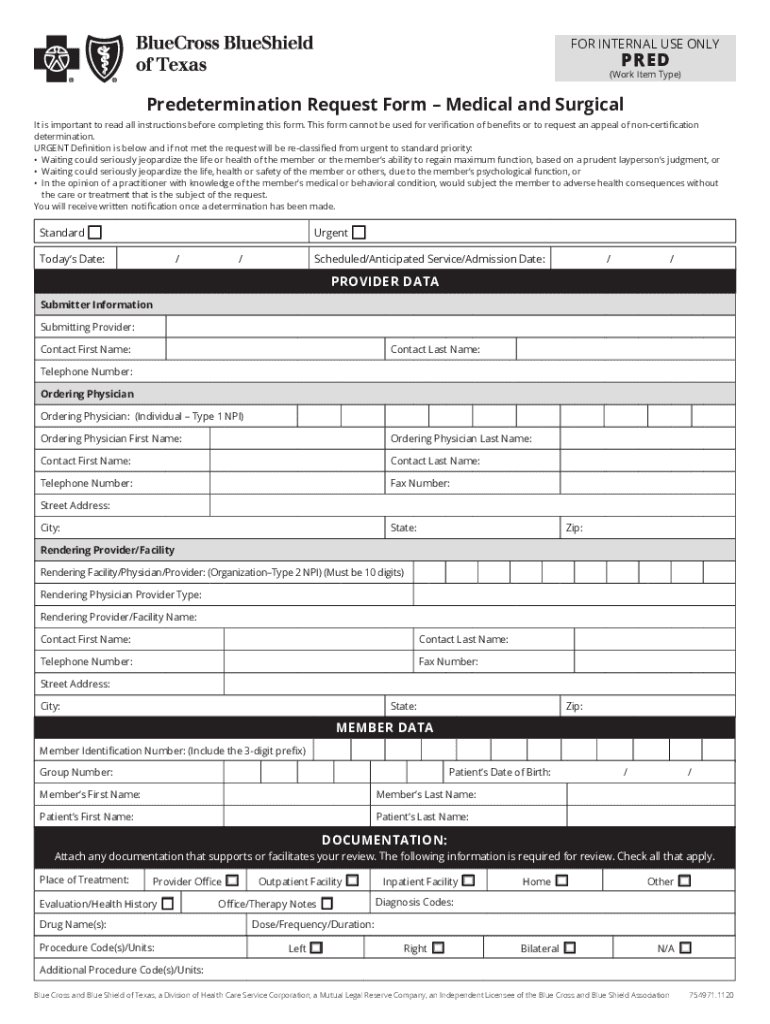
Bluecross Blueshield Of Texas Provider Appeal Request Form printable
Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. It is provided as a general resource to providers regarding the types of claim reviews and appeals that may be available for commercial and medicaid claims. Do.
Anthem Blue Cross California Grievance Form Blue Cross Blue Shield
Web here are some common forms you may need to use with your plan. If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. To help you prepare your reconsideration request, you may arrange with us to provide a copy, free of charge, of all.
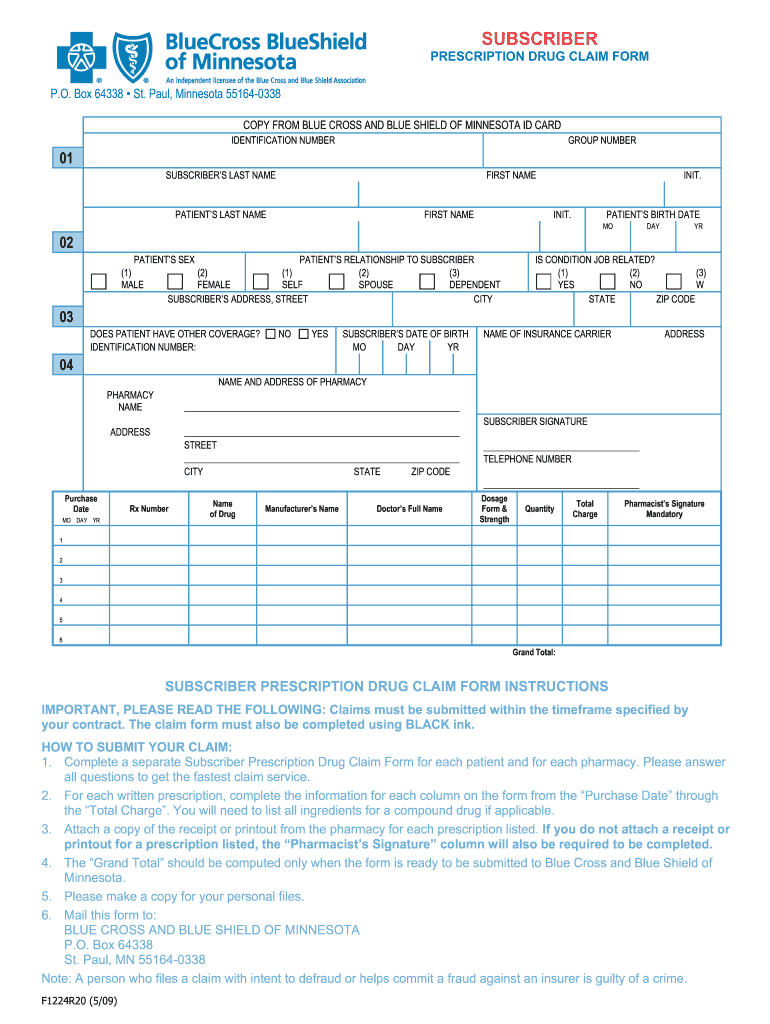
Blue Cross Blue Shield Application Form Fill Out and Sign Printable
If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. Appeals must be submitted within one year from the date on the remittance advice. You can file a complaint by phone or ask for a complaint form to be mailed to you. Do not use.
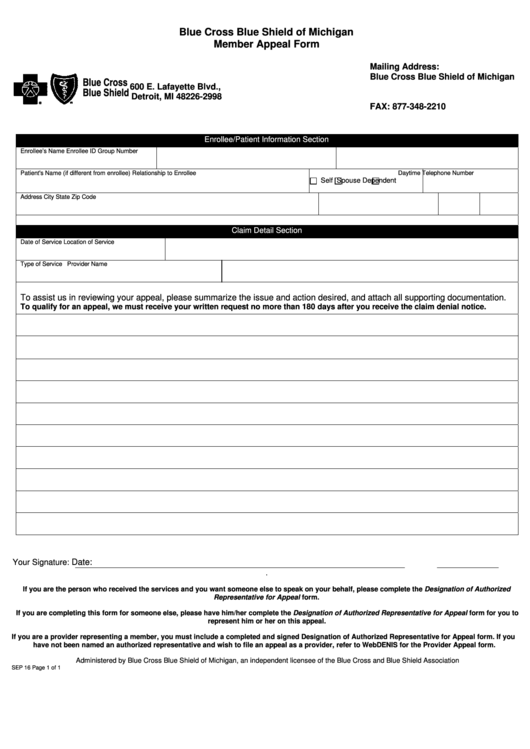
Fillable Blue Cross Blue Shield Of Michigan Member Appeal Form
Web section 8 of the blue cross and blue shield service benefit plan brochure. If you're a blue cross blue shield of michigan member and are unable to resolve your concern through customer service, we have a formal grievance and appeals process. Appeals must be submitted within one year from the date on the remittance advice. The centers for medicare.
Bcbs Federal Provider Appeal form Best Of File Plaint Blue Shield
If you have questions about a form you need, call the customer service number on the back of your member id card. Do not use this form for dental appeals. Need medicare forms or documents? If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us..
BCBSTX Home Blue Cross And Blue Shield Of Texas Fill Out and Sign
With the form, the provider may attach supporting medical information and mail to the following address within the required time. To help you prepare your reconsideration request, you may arrange with us to provide a copy, free of charge, of all relevant materials, and plan documents under our control relating to your claim, including those that involve any expert review(s).
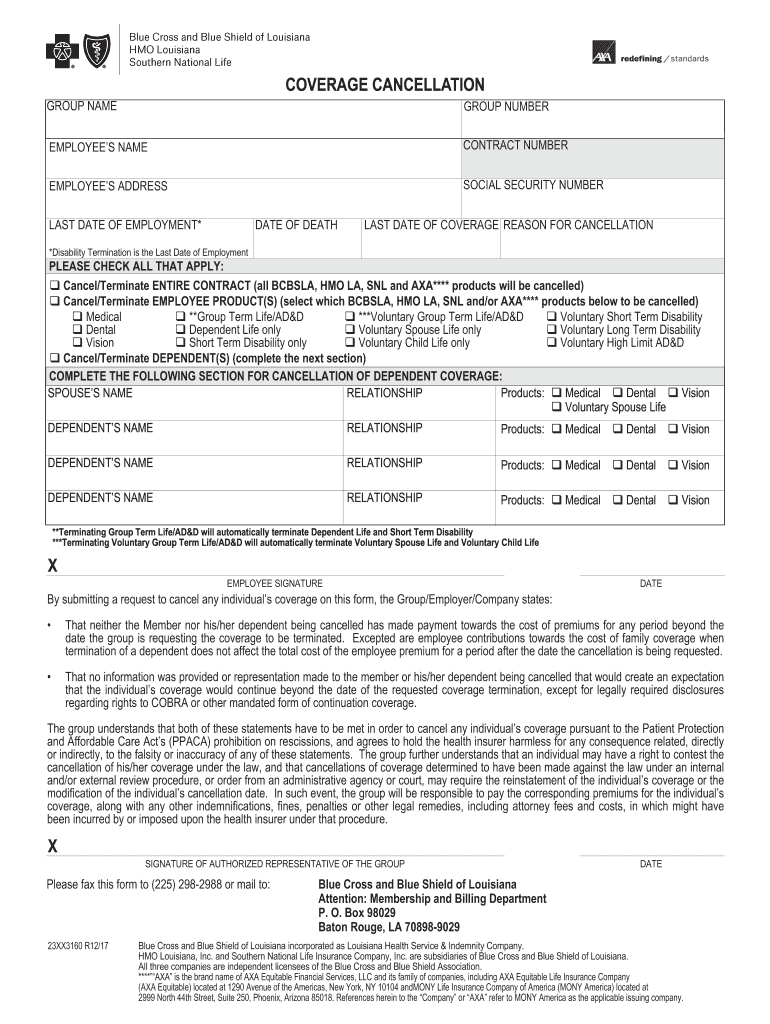
Florida Blue Cancellation Form Fill Out and Sign Printable PDF
It is provided as a general resource to providers regarding the types of claim reviews and appeals that may be available for commercial and medicaid claims. Send only one appeal form per claim. These forms can be used for coverage determinations, redeterminations and appeals. Do not use this form for dental appeals. Web claim review and appeal.
Health News » Blog Archive » Blue Cross and Blue
Web forms to use to request determinations and file appeals. Appeals must be submitted within one year from the date on the remittance advice. Web claim review and appeal. Web appeal form who is this for? Web provider appeal form please complete the following information and return this form with supporting documentation to the applicable address listed on the corresponding.
With The Form, The Provider May Attach Supporting Medical Information And Mail To The Following Address Within The Required Time.
Web forms to use to request determinations and file appeals. If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. To help you prepare your reconsideration request, you may arrange with us to provide a copy, free of charge, of all relevant materials, and plan documents under our control relating to your claim, including those that involve any expert review(s) of your claim. Web claim review and appeal.
Web Here Are Some Common Forms You May Need To Use With Your Plan.
The centers for medicare & medicaid services (cms) has developed forms for use by all blue cross medicare advantage prescribing doctors and members. The following information does not apply to medicare advantage and hmo claims. Some health plans have customized forms that are not listed on this page. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online.
If You Have Questions About A Form You Need, Call The Customer Service Number On The Back Of Your Member Id Card.
If you're a blue cross blue shield of michigan member and are unable to resolve your concern through customer service, we have a formal grievance and appeals process. Web provider appeal form please complete the following information and return this form with supporting documentation to the applicable address listed on the corresponding appeal instructions. Need medicare forms or documents? Send only one appeal form per claim.
Do Not Use This Form For Dental Appeals.
These forms can be used for coverage determinations, redeterminations and appeals. You can file a complaint by phone or ask for a complaint form to be mailed to you. Appeals must be submitted within one year from the date on the remittance advice. Web section 8 of the blue cross and blue shield service benefit plan brochure.