Blueadvantagearkansas Prior Authorization Form
Blueadvantagearkansas Prior Authorization Form - Web physician/supplier corrected bill submission form [pdf] use when submitting previously finalized (corrected) bills. Please check with your human resources office before using one of these forms. Web ***note*** a prior authorization will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with. This form authorizes the following. Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Web prior approval request form date request submitted: Referral process for primary care network; Web complete/review information, sign and date. Provider application/contract request use to request. Web 2023 prior authorization criteria (updated:
Web physician/supplier corrected bill submission form [pdf] use when submitting previously finalized (corrected) bills. Web complete/review information, sign and date. Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. View coverage policy providers' news find updates on the latest policies and. Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website. 7/1/2023) find a pharmacy (pharmacy directory) prescription claim form click here to fill out the prescription coverage. Providers who are requesting a prior approval. This review consists of checking clinical documentation to verify the. Referral process for primary care network;
View coverage policy providers' news find updates on the latest policies and. Health information network (hin) hedis measures; Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website. Web prior approval request form date request submitted: Some employers use customized forms or electronic systems. Providers who are requesting a prior approval. This form authorizes the following. Referral process for primary care network; Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Please check with your human resources office before using one of these forms.
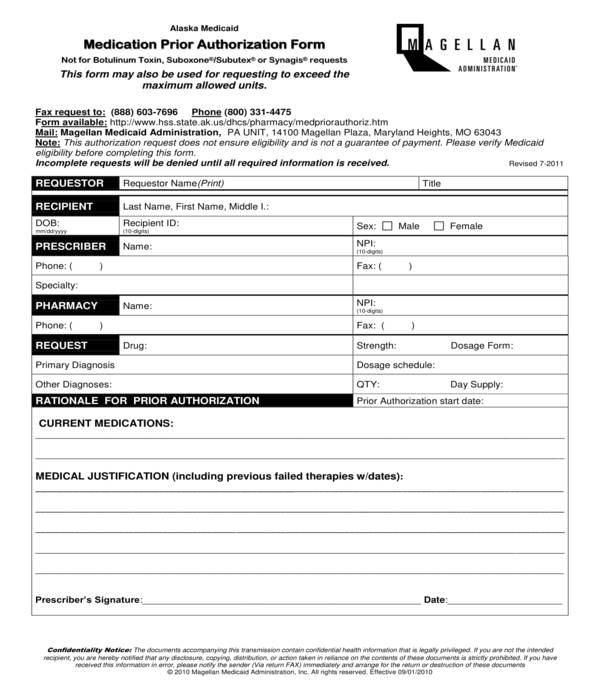
FREE 11+ Prior Authorization Forms in PDF MS Word
Web 2023 prior authorization criteria (updated: Health information network (hin) hedis measures; Providers who are requesting a prior approval. Referral process for primary care network; Web ***note*** a prior authorization will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with.
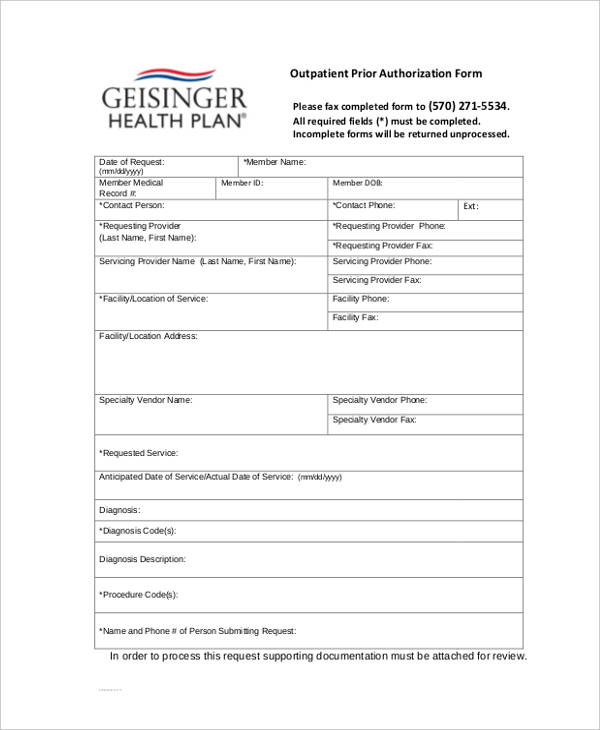
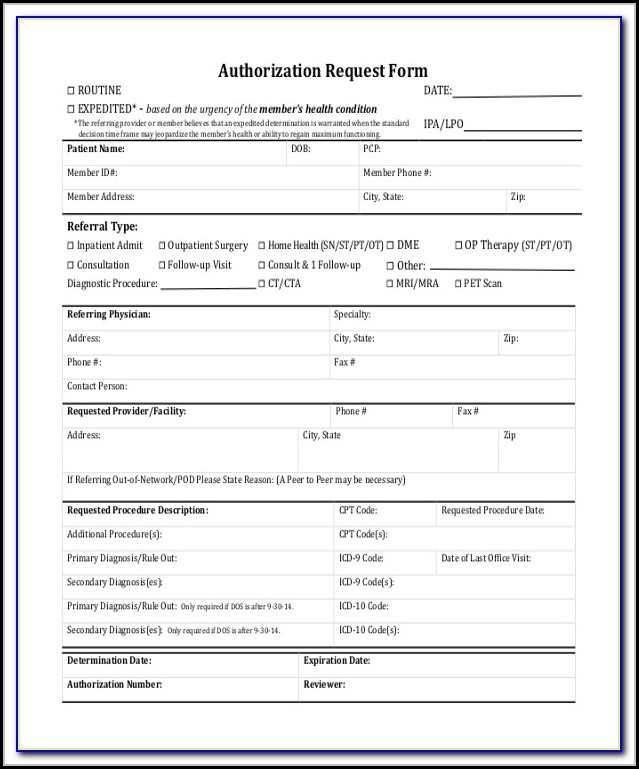
FREE 13+ Prior Authorization Forms in PDF MS Word
Health information network (hin) hedis measures; Some employers use customized forms or electronic systems. Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Please check with your human resources office before using one of these forms. Providers who are requesting a prior.
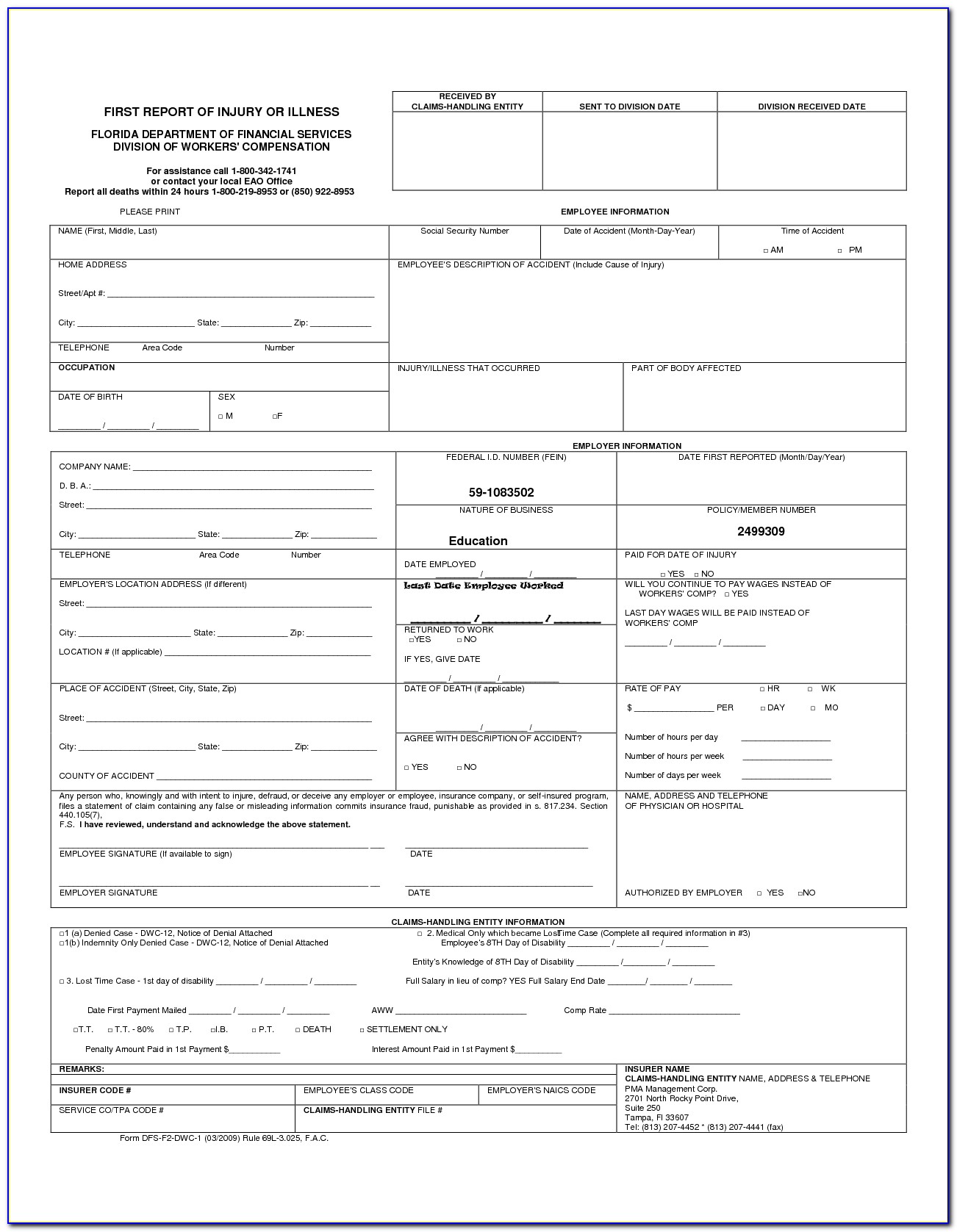
Bcbs Prior Auth Forms Florida Form Resume Examples A4kn4J95jG
Web prior approval request form date request submitted: This review consists of checking clinical documentation to verify the. Provider application/contract request use to request. Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Web 2023 prior authorization criteria (updated:
Medicare Generation Rx Prior Authorization Form Form Resume
Providers who are requesting a prior approval. Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Web prior approval request form date request submitted: This form authorizes the following. Provider application/contract request use to request.
Aarp Optumrx Prior Authorization Form Form Resume Examples EVKYM0oK06
Web 2023 prior authorization criteria (updated: Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Please check with your human resources office before using one of these forms. Provider application/contract request use to request. Web complete/review information, sign and date.
Aarp Prior Authorization Forms Form Resume Examples A19XleN94k
7/1/2023) find a pharmacy (pharmacy directory) prescription claim form click here to fill out the prescription coverage. View coverage policy providers' news find updates on the latest policies and. Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Web complete/review information, sign.
Bcbs Prior Authorization Form Form Resume Examples NRE34PV36x
Referral process for primary care network; Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. 7/1/2023) find a pharmacy (pharmacy directory) prescription claim form click here to fill out the prescription coverage. Web ***note*** a prior authorization will only be considered when.
Medicare Generation Rx Prior Authorization Form Form Resume
This form authorizes the following. Web 2023 prior authorization criteria (updated: Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Web prior approval request form date request submitted: View coverage policy providers' news find updates on the latest policies and.
Prior Authorization Form For Medicare Advantage Universal Network
Web complete/review information, sign and date. Web prior approval request form date request submitted: Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website. View coverage policy providers' news find updates on the latest policies and. Providers who are requesting a prior approval.
Bcbs Prior Authorization Form Tennessee Form Resume Examples
Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website. Provider application/contract request use to request. Some employers use customized forms or electronic systems. View coverage policy providers' news find updates on the latest policies and. Web prior approval request form date request submitted:
Health Information Network (Hin) Hedis Measures;
Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Referral process for primary care network; Web prior approval request form date request submitted:
Web 2023 Prior Authorization Criteria (Updated:
Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website. View coverage policy providers' news find updates on the latest policies and. Web complete/review information, sign and date. This form authorizes the following.
Web Physician/Supplier Corrected Bill Submission Form [Pdf] Use When Submitting Previously Finalized (Corrected) Bills.
7/1/2023) find a pharmacy (pharmacy directory) prescription claim form click here to fill out the prescription coverage. Web ***note*** a prior authorization will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with. Provider application/contract request use to request. Please check with your human resources office before using one of these forms.
This Review Consists Of Checking Clinical Documentation To Verify The.
Providers who are requesting a prior approval. Some employers use customized forms or electronic systems.