Prior Authorization Form Molina
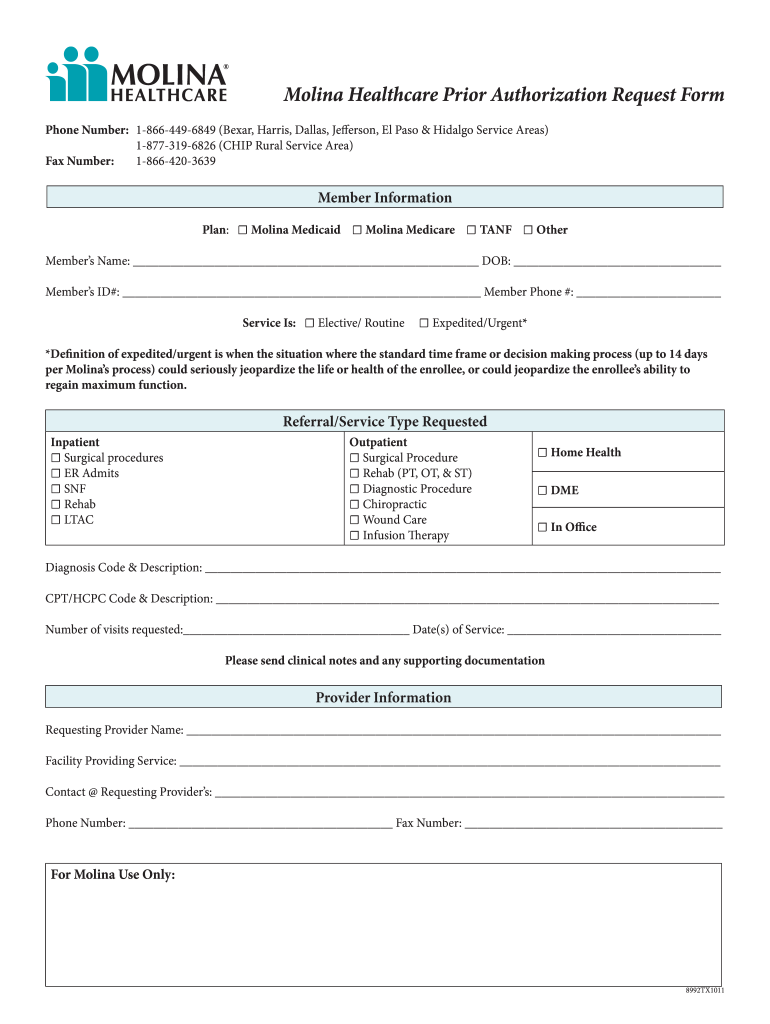
Prior Authorization Form Molina - Molina healthcare of south carolina, inc. Web effective january 1, 2022 services listed below require prior authorization. The fastest route for prior authorization is submission via fax. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid. It is needed before you can get certain. Behavioral health therapy prior authorization form. Web what are prior authorizations? Edit, sign and save prior authorization req form. It should be noted that the medical office. Web molina complete care prior authorization request form member information line of business:
Web prior authorization lookup tool. It should be noted that the medical office. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web molina complete care prior authorization request form member information line of business: Please refer to molina complete care (mcc)’s provider website or prior authorization (pa) lookup tool. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid. ☐ medicaid ☐ marketplace ☐ medicare date of request: Edit, sign and save prior authorization req form. 1/1/2020 refer to molina’s provider website.
Web effective january 1, 2022 services listed below require prior authorization. ☐ medicaid ☐ marketplace ☐ medicare date of request: Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Molina healthcare prior authorization request form and instructions. Behavioral health prior authorization form. Web prior authorization is not a guarantee of payment for services. Web molina complete care prior authorization request form member information line of business: It should be noted that the medical office. The fastest route for prior authorization is submission via fax. Molina healthcare of south carolina, inc.
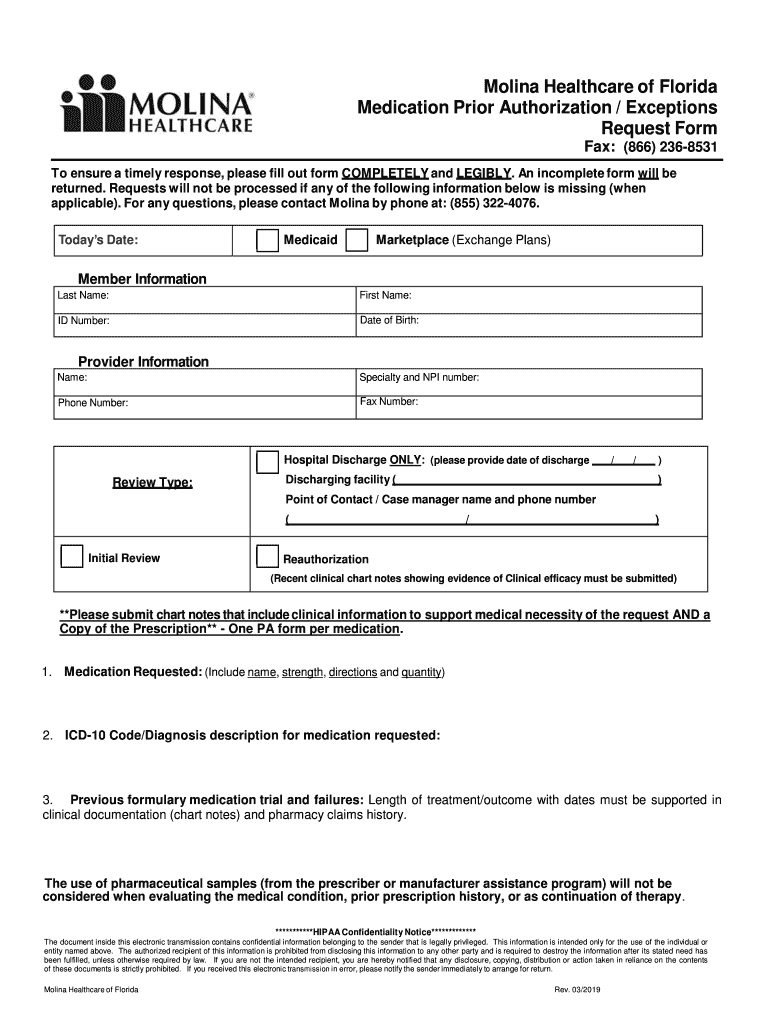
Molina Medication Prior Form Fill Out and Sign Printable PDF Template
The fastest route for prior authorization is submission via fax. Behavioral health therapy prior authorization form. Behavioral health prior authorization form. It is needed before you can get certain. Web molina complete care prior authorization request form member information line of business:
Molina Medicare Medication Prior Authorization Form Form Resume
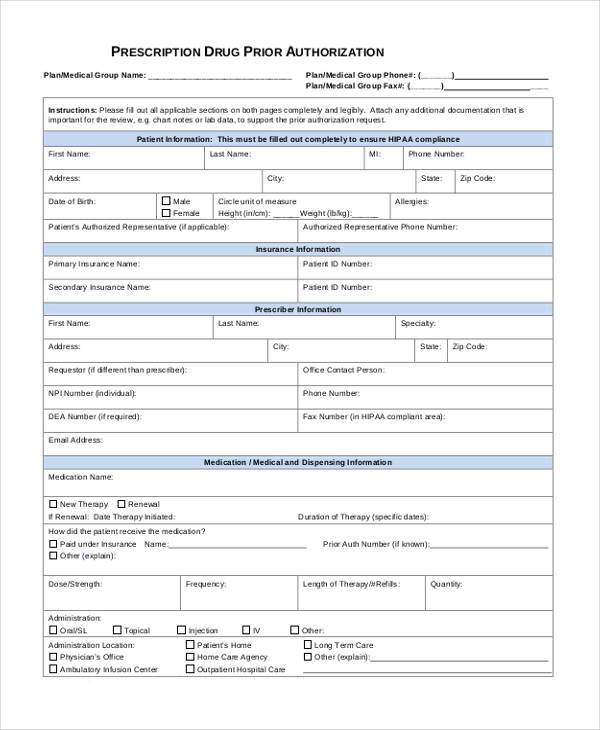
Web molina healthcare prior authorization request form and instructions nursing facility request form synagis (rsv) authorization behavioral health respite services pa. Prior authorization request contact information. Edit, sign and save prior authorization req form. Behavioral health prior authorization form. Pdffiller allows users to edit, sign, fill & share all type of documents online.
Prior Authorization Washington State Local Health Insurance CHPW
1/1/2020 refer to molina’s provider website. Pdffiller allows users to edit, sign, fill & share all type of documents online. Web prior authorization is not a guarantee of payment for services. Web effective january 1, 2022 services listed below require prior authorization. Prior authorization is when your provider gets approval from molina healthcare to provide you a service.
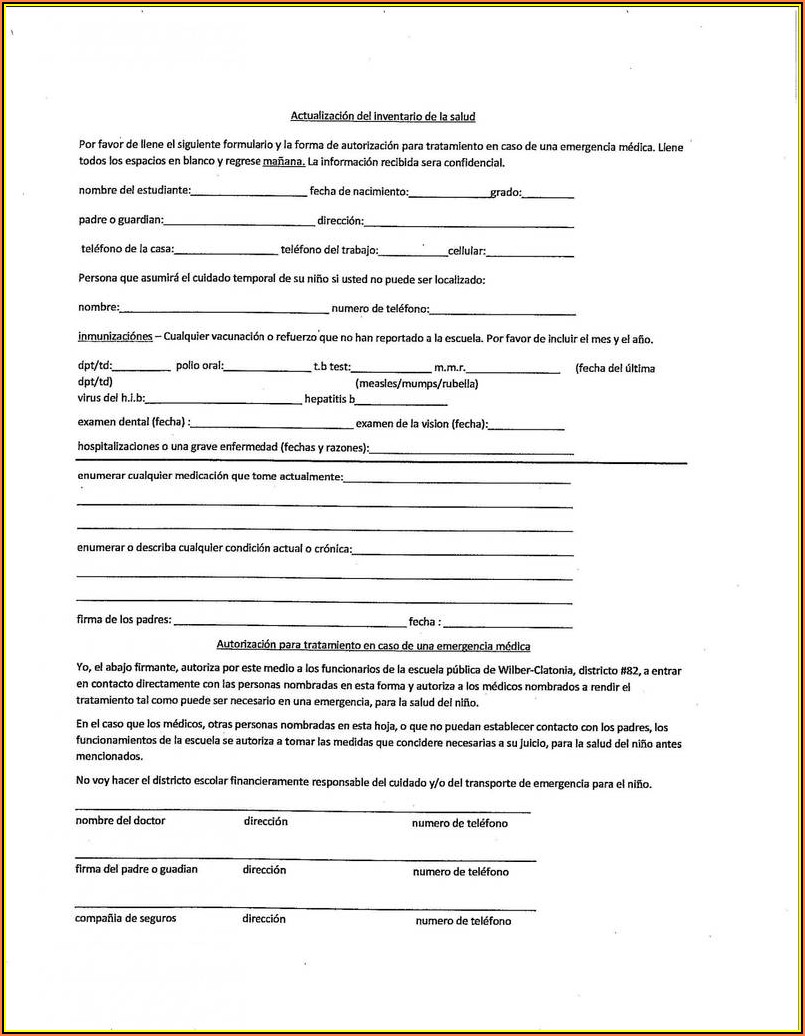
FREE 41+ Authorization Forms in PDF Excel MS word
Molina healthcare contact information prior. It should be noted that the medical office. It is needed before you can get certain. Web refer to molina’s provider website or portal for specific codes that require authorization. The quickest option for checking the status of a request is through our telephonic.
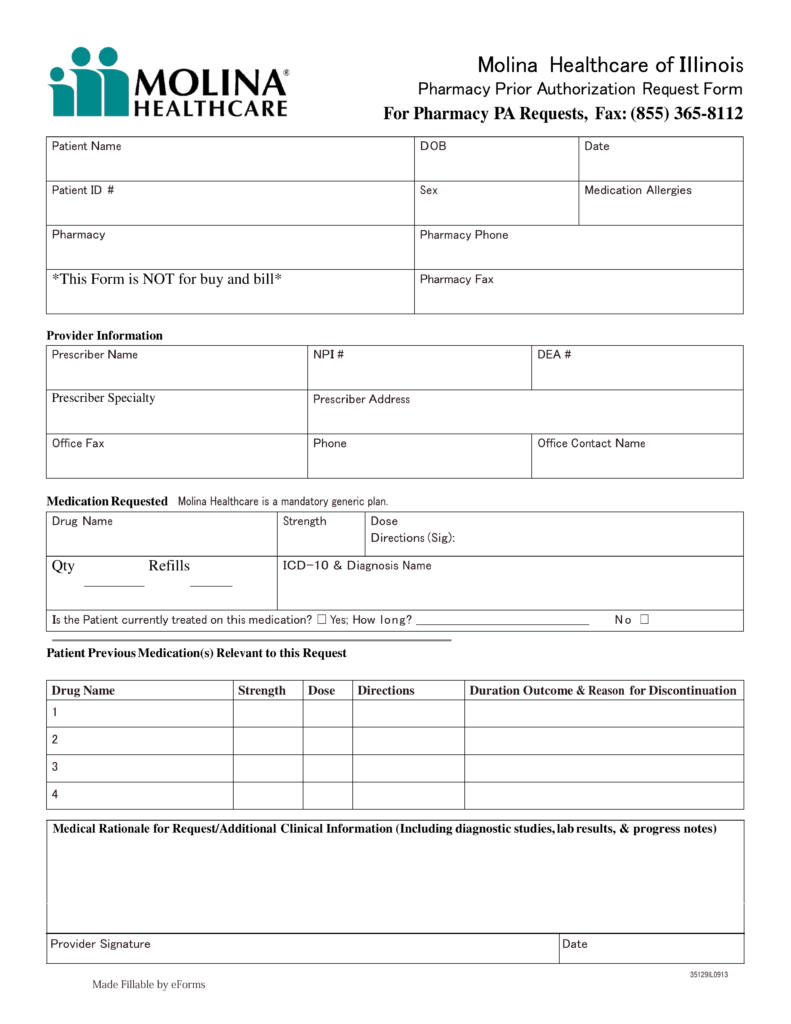
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
Molina healthcare of south carolina, inc. Please refer to molina complete care (mcc)’s provider website or prior authorization (pa) lookup tool. Web molina healthcare prior authorization request form and instructions nursing facility request form synagis (rsv) authorization behavioral health respite services pa. It is needed before you can get certain. Edit, sign and save prior authorization req form.
Molina Medicare Medication Prior Authorization Form Form Resume
Behavioral health therapy prior authorization form. Molina healthcare of south carolina, inc. Web effective january 1, 2022 services listed below require prior authorization. The fastest route for prior authorization is submission via fax. Web prior authorization lookup tool.
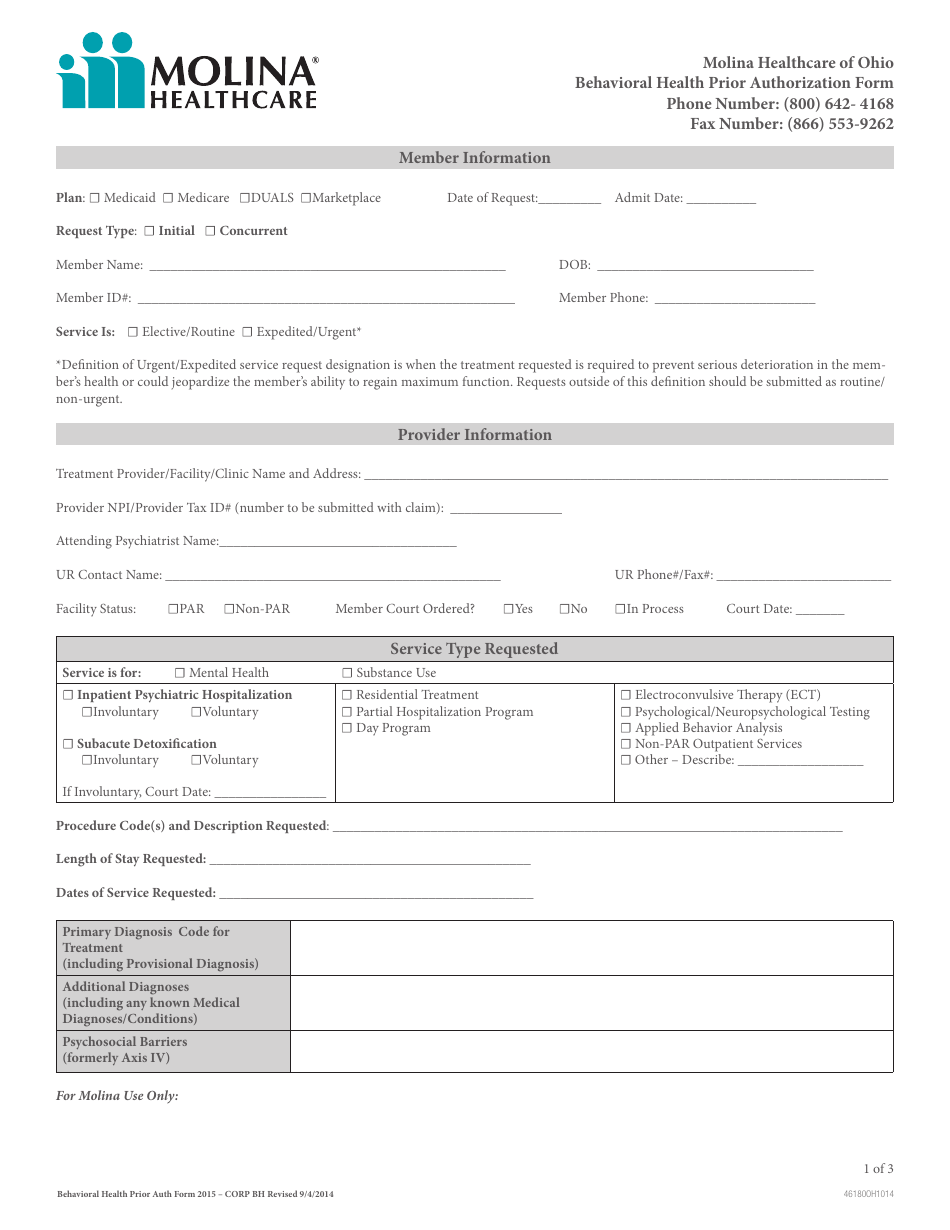
Ohio Behavioral Health Prior Authorization Molina Healthcare Download
01/01/2021 refer to molina’s provider website/prior. Molina healthcare contact information prior. Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Web prior authorization lookup tool. It should be noted that the medical office.
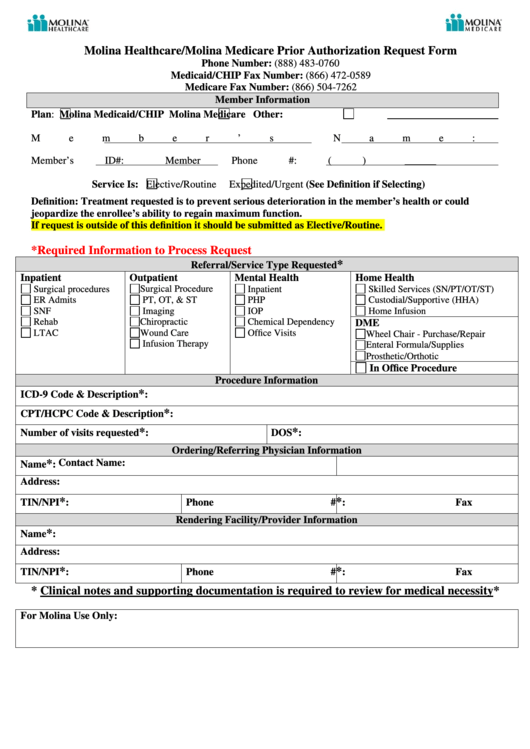
Molina Healthcare/molina Medicare Prior Authorization Request Form
Web molina healthcare prior authorization request form and instructions nursing facility request form synagis (rsv) authorization behavioral health respite services pa. Behavioral health prior authorization form. Web refer to molina’s provider website or portal for specific codes that require authorization. 01/01/2021 refer to molina’s provider website/prior. Molina healthcare contact information prior.
UT Molina Healthcare Prior Authorization Form 20162022 Fill and Sign
Web prior authorization is not a guarantee of payment for services. Behavioral health therapy prior authorization form. The quickest option for checking the status of a request is through our telephonic. Edit, sign and save prior authorization req form. Prior authorization is when your provider gets approval from molina healthcare to provide you a service.
Molina prior authorization form Fill out & sign online DocHub
Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions,. Web prior authorization is not a guarantee of payment for services. 01/01/2021 refer to molina’s provider website/prior. Web effective january 1, 2022 services listed below require prior authorization. Molina healthcare of south carolina, inc.
Molina Healthcare Contact Information Prior.
Web molina complete care prior authorization request form member information line of business: Molina healthcare of south carolina, inc. ☐ medicaid ☐ marketplace ☐ medicare date of request: It should be noted that the medical office.
Web Refer To Molina’s Provider Website Or Portal For Specific Codes That Require Authorization.
Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. The quickest option for checking the status of a request is through our telephonic. Please refer to molina complete care (mcc)’s provider website or prior authorization (pa) lookup tool.
Web Prior Authorization Is Not A Guarantee Of Payment For Services.
Web effective january 1, 2022 services listed below require prior authorization. Pdffiller allows users to edit, sign, fill & share all type of documents online. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid. Prior authorization request contact information.
Molina Healthcare Prior Authorization Request Form And Instructions.
Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions,. It is needed before you can get certain. Behavioral health therapy prior authorization form. Edit, sign and save prior authorization req form.